People have used opium and its derivatives both medically and recreationally since antiquity. However, since the early 20th century, law and society have viewed people who use opioids, cocaine, and certain other psychoactive substances as immoral and even criminal. For more than 100 years, this viewpoint has destructively intruded on the patient-doctor relationship. Government and law enforcement increasingly surveil and influence the way doctors treat pain, psychoactive substance use, and substance use disorder. This change has happened in two discernible waves, which we call Drug War I and Drug War II.
Drug War I occurred after Congress enacted the Harrison Narcotics Act in 1914, which permitted doctors to prescribe opioids to treat their patients. A wave of arrests and prosecutions of thousands of doctors ensued as agents of the U.S. Treasury Department, empowered to enforce the act, took it upon themselves to define legitimate medical practice.
Drug War II began in the 1970s, with government-funded education/indoctrination campaigns that caused both doctors and patients to fear opioids for their addictive and overdose potential. Later, as the scientific literature led medical specialty organizations and government health officials to overcome this apprehension and take the treatment of pain more seriously, opioid prescribing increased considerably.
By 2006, federal regulatory agencies perceived what they called an “opioid crisis” and mistakenly attributed it to doctors “overprescribing” opioids and generating a growing population of opioid addicts. This formed the basis for an even more massive intrusion of federal and state power into the privacy of medical records, patient-doctor confidentiality, and the very way in which doctors are allowed to use scientific and professional knowledge to practice medicine. Medical decisionmaking came increasingly under the purview of law enforcement, sparking a new wave of arrests and prosecutions.
Patients who had their pain controlled with long-term opioid treatment are being denied treatment or involuntarily tapered off their pain control, as doctors fear arrest and an end to their medical careers. A growing population of “pain refugees” has emerged, with some patients turning in desperation to the black market for opioids and some even turning to suicide. As prescribing rates continue to plunge, overdoses from the nonmedical use of opioids are skyrocketing, now largely caused by illicit fentanyl.
The medical mismanagement of pain, which causes harm to patients, is best addressed through the civil tort system. Additionally, states establish professional licensing boards specifically to enforce the “standard of care” rendered by the professionals they oversee. Law enforcement has no medical expertise and should have no say in classifying narcotics and psychoactive substances. Lawmakers should avoid passing or repeal any laws that cast in stone prescribing guidelines released by any state or federal public health agencies. Federal and state law enforcement should be required to get a warrant before perusing state prescription drug monitoring program databases. Law enforcement should be required to report any suspected standard-of-care deviations to state professional licensing boards for review and adjudication. Neither the practice of medicine nor the act of self-medication belongs in the realm of the criminal legal system.
“History doesn’t repeat itself,
but it often rhymes.”
—attributed to Mark Twain
Introduction
Why do people with alcohol-use disorder get treatment while heroin users get put in cages or a different form of criminal punishment? This question is at the heart of our drug policies both historically and currently, and critically examining the answer will help us be more compassionate and helpful to our fellow drug-using human beings. We use the phrase “human being” quite deliberately. Our drug policies systematically dehumanize the users of some psychoactive compounds. Those who use heroin have been regarded as “junkies” whose drug use is more morally suspect than those who use substances such as alcohol or marijuana. That differential moralizing of different substance users is, fundamentally, why we give alcoholics treatment and heroin users criminal punishment: we tend to like alcoholics more, and more of us have personal experience with alcohol.
This paper examines the history of the dehumanization of opioid users and the demedicalization of opioids as drugs that doctors, in their expertise and judgment, use to treat various ailments, particularly chronic pain and substance use disorder. Together, these two phenomena have drastically changed the relationship between doctors and patients.1 Since the early 20th century, the relationship between doctors and patients who use opioids has changed consistently, along with government control over that relationship. Law enforcement officials increasingly surveil and influence the way doctors treat pain, psychoactive substance use, and substance use disorder. This has occurred in two discernible waves that we call Drug War I and Drug War II (see Appendix for timeline of events).
During Drug War I, in the first half of the 20th century, a wave of arrests and prosecutions of doctors occurred under the Harrison Narcotics Act of 1914. Originally a relatively benign tax act, in the hands of Treasury agents it became a de facto prohibition. Treasury agents took it on themselves to define legitimate medical practice, and thousands of doctors were prosecuted.
Drug War II began in the 1970s, as government-funded education/indoctrination campaigns began to instill a fear of opioids among doctors and patients alike. In many cases, doctors and patients feared opioids for different reasons. This “opiophobia” caused many patients to suffer needlessly. Doctors feared that prescribing opioids might turn their patients into addicts. Even worse, doctors worried that prescribing opioids liberally might lead to their arrest and loss of their license to practice.2
Reacting to multiple studies in the peer-reviewed scientific literature along with admonitions from government health officials and medical specialty organizations, doctors and patients became less apprehensive about treating pain with opioids, and opioid prescribing increased considerably by the late 1990s.3
Originally attracting the attention of federal regulatory agencies in 2006, what would soon be known as the “opioid crisis”—a surge in overdose deaths from the nonmedical use of prescription opioids and illicit drugs, particularly among adolescents and teens—formed the basis of the second, more massive wave of intrusion of federal and state power into the privacy of medical records, patient-doctor confidentiality, and the very way in which doctors are allowed to use scientific and professional knowledge to practice medicine.4 Medical decisionmaking is increasingly under the purview of law enforcement. Practitioners and patients alike are often prejudged as criminals. Patient and professional autonomy is under assault. Professional organizations revised their pain management recommendations as the pendulum swung back toward opiophobia.5
The U.S. Drug Enforcement Administration (DEA) sets strict quotas on the types and amounts of prescription opioids that individual manufacturers may produce to serve the entire population in a given year, and it has been intentionally drawing them down, sometimes causing national shortages.6 State governments impose strict limits on the dosages and number of opioids that health care practitioners may prescribe to patients in pain under various clinical circumstances. The prescribing habits of providers, as well as the medication histories of patients, are kept under close surveillance by prescription drug monitoring programs, with law enforcement investigating and prosecuting providers who are deemed to deviate from a state-defined norm. Criminal prosecutions and license revocations intimidate doctors, pharmacists, and other health care practitioners into modifying their treatment decisions to comply with state-mandated standards. Law enforcement personnel search state-based prescription databases for “overprescribing” practitioners.
In the process, many acute pain patients now go undertreated or even untreated for acute pain, while chronic pain patients become desperate as their doctors abruptly taper or cut them off the pain medications on which they have been relying to lead a productive and meaningful life. Many resume a homebound or bedridden existence, while others look to the black market or suicide for relief.7 In some, an adversarial relationship develops between patient and doctor because patients believe their doctors are not taking their pain seriously.8 There are mounting press reports of angry and dissatisfied pain patients threatening their doctors and, in extreme cases, becoming homicidal.9 Some chronic pain patients whose doctors’ practices have been shuttered by government authorities find themselves without a doctor and with no other doctor willing to take the legal risk of assuming their care. These “pain refugees” wander from doctor to doctor in search of relief, often getting tagged by surveillance teams as “doctor shoppers” because of multiple prescriptions obtained from various practitioners.10
The “opioid crisis” has resulted in patients and practitioners losing privacy and autonomy as the state has assumed control over the diagnosis and treatment of acute and chronic pain. Many practitioners are losing their licenses or facing incarceration for “overprescribing” pain medication, with no clear and universally accepted definition of “overprescribing.”11 Fourteen years after the opioid crisis was proclaimed, there is no sign it is receding.
Drug War I: The Harrison Narcotics Act and the Illegal Persecution of Doctors
Medical provision of opioids was a central element of the first major federal drug law, the Harrison Narcotics Act of 1914. That law was designed to bring transparency to the opioid market and to restrict opioid distribution to certain licensed professionals such as doctors and pharmacists. In the hands of the federal revenue agents who were charged with enforcing the act, however, the law became a de facto prohibition, and those doctors who thought their medical opinions would carry weight found themselves facing prosecution for overprescribing or prescribing to prohibited persons (such as compulsive opioid users).
The Harrison Narcotics Act was not supposed to be the straight-up prohibition statute it became. For a few years after the law was passed, clinics were set up in various cities around the country that catered to compulsive users who no longer had reliable access to opioids. That experiment in compassionately providing opioids to compulsive users—users who often had developed dependence when opioids were widely available without a prescription—was quickly shut down by overzealous federal agents with a prohibitionary mindset. What followed was an era of doctors being imprisoned and prosecuted for acting on their medical opinions.
Opioid Use in the Late 19th and Early 20th Centuries
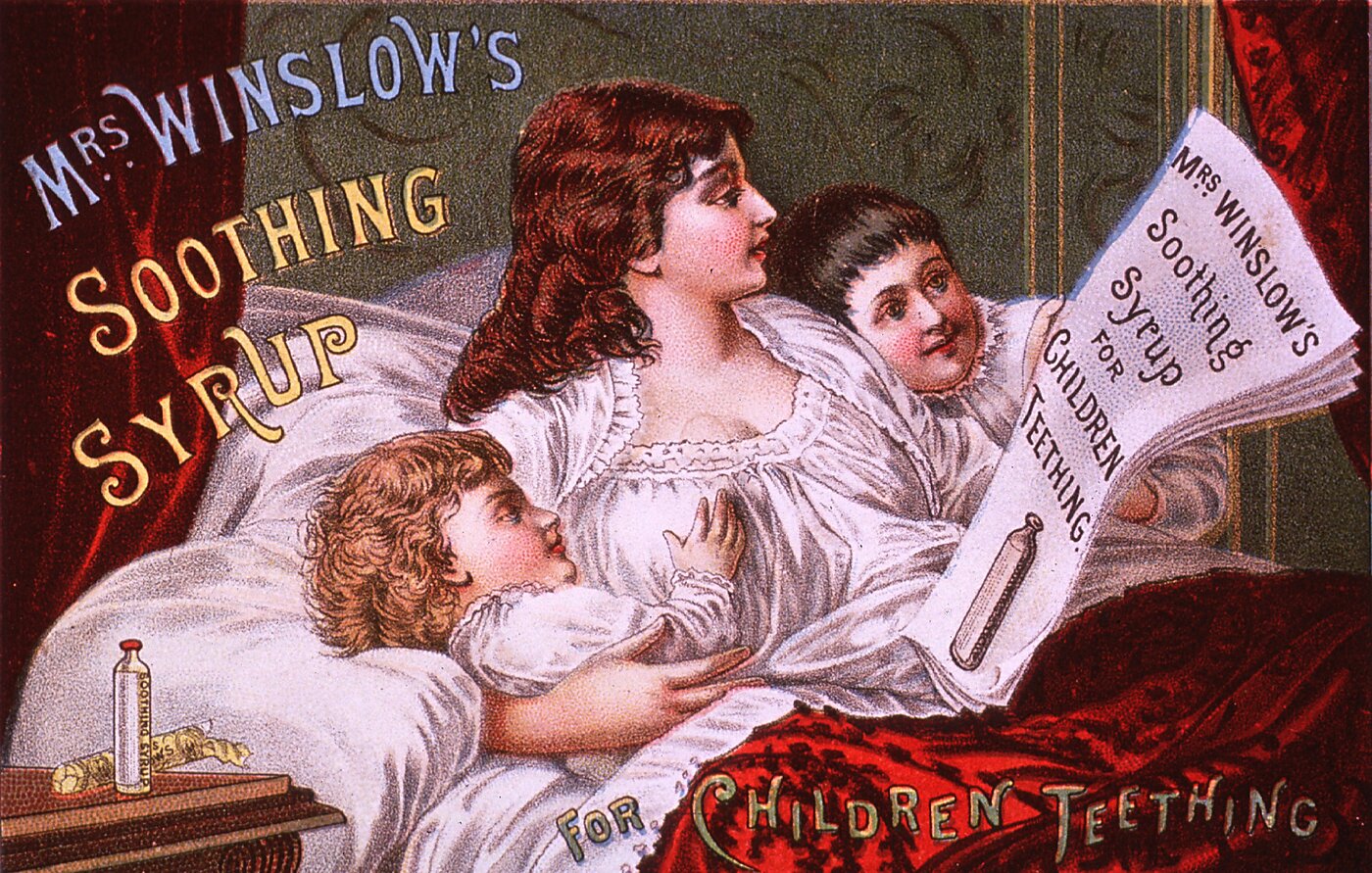
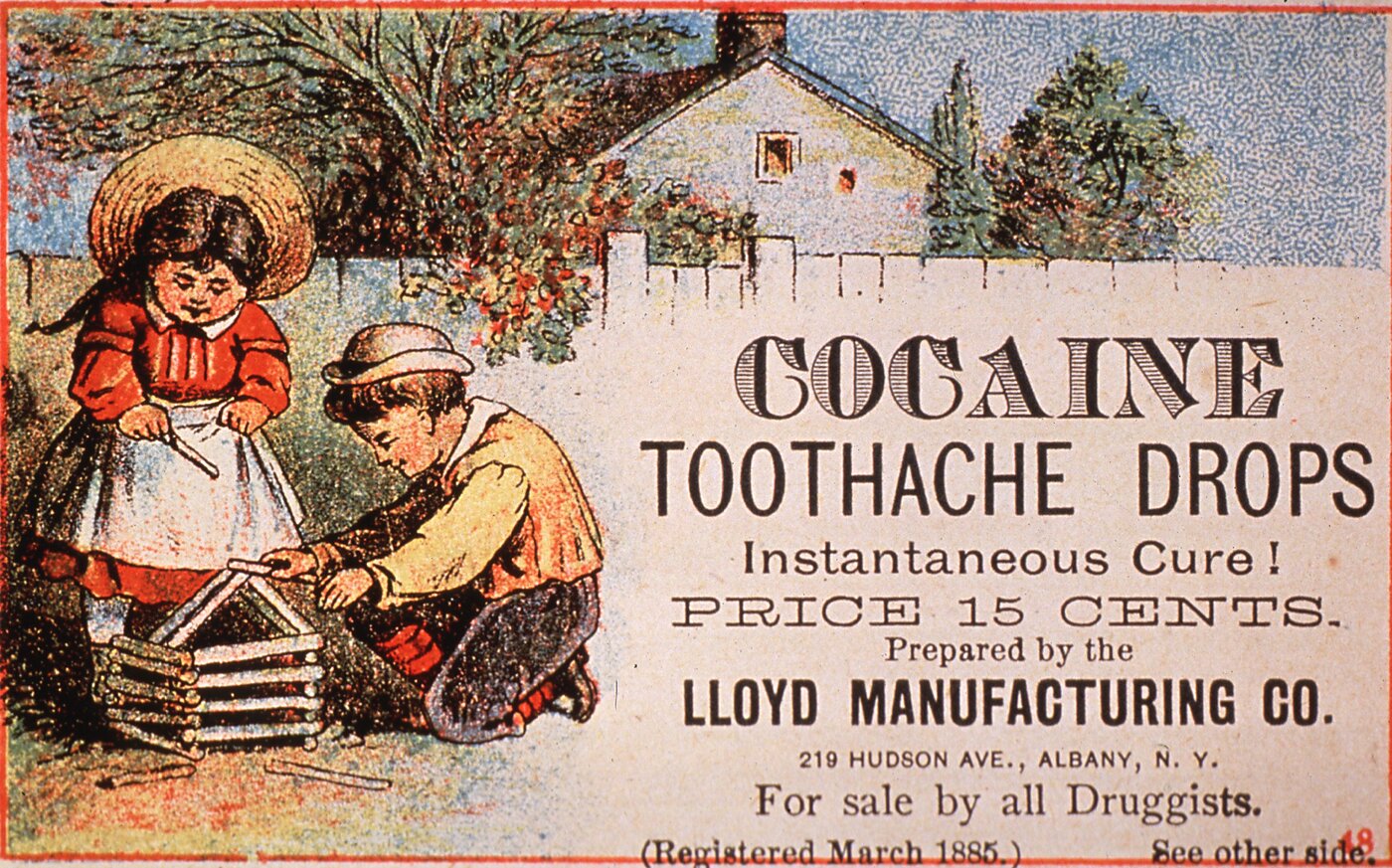
Today, opium prohibition seems almost natural, inevitable. Yet opium and its derivatives were broadly legal in the United States before 1914. Americans could buy opium-based products off the shelf. Those products took many forms, including tinctures, soothing syrups, numerous “patent medicines,” and laudanum (usually a mixture of alcohol and opium).12
The image of the opioid user was entirely different in the late 19th century from today. Doctors prescribed opium for many ailments because it often helped, especially compared with what else was available. Opium has long been a well-known cough suppressant—as it is still used today—and given the number of common diseases for which coughing is a symptom, it’s unsurprising that it was commonly prescribed. But it was thought to be useful for other things. One 1880 medical text—Dr. H. H. Kane’s The Hypodermic Injection of Morphia: Its History, Advantages, and Dangers (Based on the Experience of 360 Physicians)—listed 54 diseases that could be treated by morphine.13 And of course many took opioids to alleviate various forms of pain, much as we take Percocet or Vicodin today.
Outside of a doctor’s office, many people found that taking various forms of opioids helped soothe their nerves and calm their anxieties, similar to how antidepressants such as Prozac and anxiety-relief medications such as Xanax are used today. Opioids helped people deal with maladies that are now listed on drug commercials: social anxiety disorder, sleeplessness, panic attacks, and so forth. An American Textbook of Applied Therapeutics of 1896 said that opioid users took the drugs to “soothe their shattered nervous systems.”14
Today, many regard the idea of opioids serving a legitimate anti-anxiety function as quixotic and dangerous. Yet for millions of people today, as back then, that is opioids’ primary function. In a 1956 study of addicts in Vancouver, British Columbia, 71 heroin addicts were asked to check boxes describing how heroin made them feel. Only 8 checked “thrilling,” and 11 checked “joyful” or “jolly.” Sixty-five reported that heroin “relaxed” them, and 53 said it “relieved worry.”15
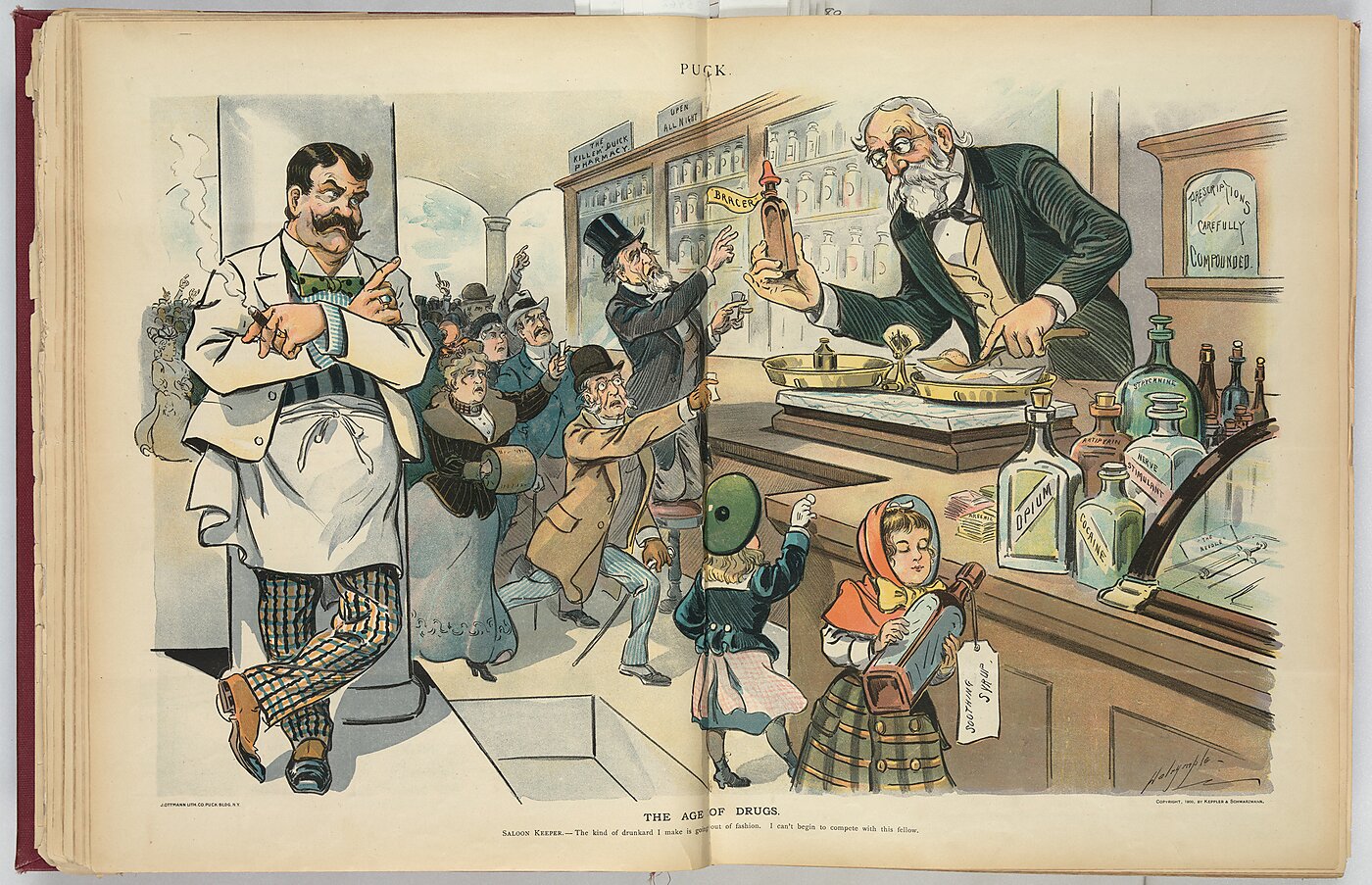
Yet then, as today, there were many who were chemically dependent on opioids. But opioid users of the time were usually regarded as less morally reprehensible than those who habitually consumed “demon rum” in saloons, burning through their paychecks night after night and leaving their families destitute. Opium users with a reliable supply could be, and often were, upstanding members of society. As long as they could maintain a supply, opioid addiction did not necessarily entail almost any of the imagery we associate with users today: gaunt, pale, sickly “junkies” willing to do anything to get the next fix.
In fact, in the late 19th century, opium users were mostly women. An 1878 Michigan survey found that 61.2 percent of self-reported users were women, and an 1880 Chicago study found that women users outnumbered men by a 3 to 1 ratio.16
The image of an unfortunate opium addict was perhaps best encapsulated by the character Mary Tyrone in Eugene O’Neill’s Long Day’s Journey into Night. O’Neill’s starkly autobiographical play has Mary struggling with a longtime morphine addiction that arose from a difficult childbirth, mirroring O’Neill’s real mother’s struggle with the drug. Mary is not treated as a criminal, however, but as a sympathetic character in a haze throughout the play, much to her family’s disconcertion. Her morphine addiction is certainly treated as a lamentable vice, but locking her up would have been regarded as absurd.

Advertisement from 1892 for “Opium and Morphine Habit Cure,” promoting the World’s Columbian Exposition in Chicago, Illinois.
Addiction was regarded as the biggest drawback of opioid use, and it could be regarded with moral opprobrium. Yet opium addicts—or habitués as they were often called—were not shunned to the degree that would later occur. At worst they were regarded as fallen human beings, and as such they did not deserve to be stepped on. In the words of one commentator:
But while deemed immoral, it is important to note that opiate use in the nineteenth century was not subject to the moral sanctions current today. Employees were not fired for addiction. Wives did not divorce their addicted husbands, or husbands their addicted wives. Children were not taken from their homes and lodged in foster homes or institutions because one or both parents were addicted. Addicts continued to participate fully in the life of the community. Addicted children and young people continued to go to school, Sunday School, and college. Thus, the nineteenth century avoided one of the most disastrous effects of current narcotic laws and attitudes—the rise of a deviant addict subculture, cut off from respectable society, and without a “road back” to respectability.17
This is not meant to paint an unrealistically rosy picture of past opioid use. There were many who were chemically dependent, and people were understandably alarmed by the number of compulsive users in the country (even if those numbers were often inflated). During the first decades of the 20th century, the drug took on an increasingly negative image. Consequently, the compulsive opioid user also took on that image, and addiction came to be regarded as a moral failing worthy of condemnation and criminal punishment.
What changed?
The Harrison Narcotics Act
Various states began banning or regulating over-the-counter opioids in the first decades of the 20th century, and after the federal Harrison Narcotics Act, opioids essentially disappeared from the shelves.18 Millions of chemically dependent users were deprived of an easy and reliable source of satiation for their habit, and many predictably moved into the illegal market. Although prohibition may take away easy-access sources for drugs, it does not magically fix chemically dependent users.
The Harrison Act was the first significant federal drug law in the United States and, as amended, was the basic federal drug law for 56 years until the Controlled Substances Act was passed in 1970. There were earlier laws, such as the Opium Exclusion Act of 1909 that regulated the importation of opium, but the Harrison Act was the first to domestically regulate the sale and possession of opium and its derivatives.
The push for the Harrison Act came primarily from the State Department. Opium had become a matter of increasing international concern. During the International Opium Convention of 1912 in The Hague, the United States had taken a lead role in both organizing the convention and pushing other countries to sign an international agreement on opium control.19 The convention was a promise from participating nations to use their “best endeavours to control” the manufacture, sales, and importation of opiates and cocaine.
But the United States did not yet have a federal drug law and thus couldn’t claim to be using its “best endeavours” to control narcotics. That gave the country less legitimacy when it badgered other countries to sign the International Opium Convention and control narcotics within their borders. Hamilton Wright—a major player for the United States at the convention and a vehement opponent of drugs—was thus determined to pass some sort of federal legislation on drugs.20
The Harrison Act was the product of many negotiations and compromises with the interested parties—namely drug manufacturers, physicians, and pharmacists. Proposed record-keeping requirements were relaxed at the request of physicians, certain tinctures and serums containing low levels of opium were exempted, and drugs were not taxed by weight. A provision was even inserted that protected the practice of physicians sending prescribed opioids by mail to those who described their symptoms in a mailed-in form. Much to Wright’s dismay, the Harrison Act protected opioids and cocaine that had been “prescribed in good faith by a physician, dentist, or veterinary surgeon registered under this Act.”
In short, the Harrison Act was not intended to completely prohibit opioid sales and use. Even after it passed, in the words of historian David Musto, “the practical significance of [the Act] was still debated among the groups affected” and “there was no general agreement on what would be the desirable or actual enforcement of the law.”21 But the senators and members of Congress who voted for it could not have read the language of the act to constitute an outright ban on opioids. The act only became a de facto ban after it was given to zealous enforcers—that is, the Treasury Department—who went after opioid users with the same progressive and moralistic fervor that lay behind the movement for alcohol prohibition.
By its text, the act created mild registration and record-keeping requirements that were seemingly far and away from a “drug war.” Those who manufactured or distributed opioids and cocaine were required to register with the local tax collector and pay $1 per year. Registrants were then issued forms—the price of which would be set by the IRS “but shall not exceed the sum of $1 per hundred”—that would have to accompany every transfer of the regulated substances.22
The text of the act doesn’t even mention “addicts” because the word had not yet become widely used. It does mention “patients” and exempts doctors who comply with a few requirements that are worth noting in full for how innocuous they are:
Nothing contained in this section shall apply … to the dispensing or distribution of any of the aforesaid drugs to a patient by a physician, dentist, or veterinary surgeon registered under this Act in the course of his professional practice only: Provided, that such physician, dentist, or veterinary surgeon shall keep a record of all such drugs dispensed or distributed, showing the amount dispensed or distributed, the date, and the name and address of the person to whom such drugs are dispensed or distributed; except such as may be dispensed or distributed to a patient upon whom such physician, dentist, or veterinary surgeon shall personally attend; and such record shall be kept for a period of two years from the date of dispensing or distributing such drugs, subject to inspection, as provided in this Act.23
All evidence shows that Congress intended for opioid users to be able to get appropriate relief from those doctors who had properly registered under the act and complied with the modest requirements. A doctor, in the “course of his professional practice,” could prescribe opioids in accordance with his medical opinion. The primary concern was identifying and stopping “pushers” and “peddlers,” those who dispensed opioids without “personally attend[ing]” to patients—in the words of the law—and didn’t maintain adequate records and tax payments.
The Public Health Service confirmed that intention in a letter to a morphine-addicted woman who wrote to the service of her worries that her supply would be cut off by the act. The surgeon general’s response assured her that the act would not cut off her supply because she would still be able to get it from her physician. The act was designed only to collect information, he said.24
According to Hamilton Wright, the act was designed to move the drug trade into visible channels and then activate public opinion against opioids:
It is designed to place the entire interstate traffic in the habit-forming drugs under the administration of the Treasury Department. It is the opinion of the American Opium Commission that it would bring this whole traffic and the use of these drugs into the light of day and thereby create a public opinion against the use of them that would be more important, perhaps, than the Act itself.25
Although some, like Wright, had long crusaded against opioid use, many understood that the compulsive opioid user was an unfortunate character who may have become addicted via medical prescription or perhaps by using laudanum as a sleep aid a little too often. If someone became a compulsive user while opioids were still available on store shelves, it seemed wrong to simply cut them off. Like alcoholics are viewed by many today, such users deserve compassion and understanding rather than punishment.
The First War on Physicians: Enforcing the Harrison Narcotics Act
As the Harrison Act was ostensibly a tax act, the job of enforcement went to the Bureau of Internal Revenue. At that time the income tax was new—the 16th Amendment authorizing an income tax had been ratified in 1913—and the Bureau of Internal Revenue had been historically in charge of chasing down smugglers who evaded various taxes on goods. Yet the scope of registering and monitoring the domestic opioid business was quite vast, on a scale unlike anything the bureau had done before. By the end of June 1916, 124,000 doctors, 47,000 pharmacists, and 37,000 dentists were registered.26
As with many laws, parts of the Harrison Act had to be interpreted by the enforcing agency. The Treasury Department issued further clarifications and definitions on March 9, 1915. In those regulations the act began to take on a different, more prohibitionary character. Physicians were told that the act’s requirement to “personally attend” to those who were prescribed opioids would be interpreted to require the physician, dentist, or veterinarian to “actually be absent from his office and in personal attendance on a patient”—in other words, a house call. The Treasury Department also decided to limit those who could register under the act to certain professions, meaning that mere consumers could not apply. Thus, possession of opioids obtained through an unregistered channel would be prima facie evidence of a crime, and the burden would be on the possessor to prove the drugs were obtained legally.
In the initial months after enforcement began, confusion abounded. One druggist wrote to the attorney general in May 1915, seeking guidance on dealing with revenue agents who were hounding him for prescribing too much. Despite administering the prescribed amount of cocaine to six users—an amount believed by the prescribing physician to be correct for those users—the druggist was confronted by “revenue agents who are neither lawyers nor physicians tell[ing] [him] that these prescriptions are in excessive amounts.” (If the druggist were alive today, he could share his grievances with doctors and pharmacists who are told by DEA agents they are “overprescribing” opioids to patients.) The druggist was flummoxed, and he sought a “straight-out, clear-cut answer and not a vague one that will leave us to our own opinions and the resulting friction with different inspectors.” In reply, the attorney general offered no help, saying the interpretation of the limits of prescribing was “a proper matter for the determination of the judiciary.”27
Yet the Treasury Department wasn’t as deferential to the judiciary as the Department of Justice. Rather than wait for the judiciary to offer a statutory interpretation of the words “in the course of his professional practice only,” the Treasury moved forward with a regulation that put physicians and pharmacists on notice that prescribing practices would be carefully monitored to see if drugs were given to compulsive users to maintain their habits:
Therefore where a physician, dentist, or veterinarian prescribes any of the aforesaid drugs in a quantity more than is apparently necessary to meet the immediate needs of a patient in the ordinary case, or where it is for the treatment of an addict or habitué to effect a cure, or for a patient suffering from an incurable or chronic disease, such physician, dentist, or veterinary surgeon should indicate on the prescription the purpose for which the unusual quantity of the drug so prescribed is to be used. In cases of treatment of addicts these prescriptions should show the good faith of the physician in the legitimate practice of his profession by a decreasing dosage or reduction of the quantity prescribed from time to time, while, on the other hand, in cases of chronic or incurable diseases such prescriptions might show an ascending dosage or increased quantity.28
But many lawyers in the Department of Justice were not so sanguine that federal judges would agree with that interpretation of the Harrison Act. The statute, after all, did not define the terms “professional practice” or “good faith.” Moreover, under the prevailing constitutional interpretation of the time—and still to some extent today—Congress lacked the power to directly regulate the medical profession. Some judges felt that the Harrison Act, on its face a tax but with far-reaching implications for how doctors practiced medicine, came perilously close to unconstitutionally regulating the medical profession. If, on the one hand, the law left the terms “professional practice” and “good faith” to be defined by state medical licensing boards and disciplinary committees, then the Harrison Act merely taxed a product without interfering in the actual practice of medicine. If, on the other hand, the federal government was going to meddle in the prescribing practices of doctors, then the law looked more like a direct regulation of the medical profession that was likely unconstitutional.
The Supreme Court Weighs In
The Harrison Act was framed as a registration and tax act for constitutional reasons. In 1914, before the Supreme Court greatly expanded congressional power in a series of decisions in the 1930s, Congress was generally thought to lack the power to either prohibit drugs or regulate the medical profession. Those powers resided primarily with state and local governments, and Congress could constitutionally reach only those things that counted as “interstate commerce.” This was why, for example, nationwide alcohol prohibition required a constitutional amendment rather than a simple statute. The 18th Amendment prohibited alcohol and expanded Congress’s powers to enforce the ban because, under the Constitution as understood at the time, Congress lacked the power to directly prohibit or regulate alcohol within a state.
But Congress did have the power to tax, and that power, at least in 1914, was considered much broader than Congress’s power to directly regulate under the Interstate Commerce Clause. Yet there were still some lingering questions about the scope of Congress’s taxing power. For example, could it use a high tax to essentially create a de facto prohibition? If Congress lacked the power to prohibit alcohol, what if it just taxed it at $10,000 per ounce? Or would that be illegitimate because Congress would essentially be using a constitutional back door to pass a prohibition?
The first challenge to the Harrison Act reached the Court in December 1915, just nine months after the law went into effect. Treasury agents had spent those months often frustrated at the reluctance of Department of Justice attorneys and federal judges to endorse their interpretation of the act. Treasury officials wanted to prosecute doctors and druggists for prescribing maintenance doses to addicts, and they also wanted to prosecute users for possessing opioids without being registered under the act. Yet judges across the nation disagreed with the Treasury Department’s interpretation. On its face, it seemed the law did not allow for second-guessing a doctor’s good-faith medical opinion. Judges also dismissed cases against users who were prosecuted for not being registered. Because the act limited registration to certain professions, a user could not be prosecuted for not being registered if he was not permitted to register in the first place.
Those issues first went to the Supreme Court in the case of United States v. Jin Fuey Moy. Dr. Jin Fuey Moy of Pittsburgh was charged with conspiracy to violate the Harrison Act when he prescribed 1 dram of morphine sulphate (about 1.8 grams) to a compulsive user named Willie Martin. Dr. Moy allegedly “did not issue [the prescription] in good faith, but knew that the drug was not given for medicinal purposes but for the purpose of supplying one addicted to the use of opium.”29
The Court decided that Martin, not being a producer, importer, manufacturer, or dealer of opioids, could not be charged with failing to register under the act, as the act did not permit him to register. Dr. Moy’s indictment for conspiring with Martin was thus illegitimate. The justices did not reach the constitutional issue because the case was decided on narrower grounds. They did acknowledge, however, that an overly broad reading of the act encompassing every person in the country rather than certain professions—in other words, users like Martin—would create constitutional issues, because Congress could not have “meant to strain its powers almost if not quite to the breaking point in order to make the probably very large proportion of citizens who have some preparation of opium in their possession criminal.”30
The Supreme Court addressed the constitutional question head-on four years later in United States v. Doremus. This time the Court considered whether Congress could use its taxing power as a back door to regulating drugs, something it could not do directly. By a narrow 5–4 vote, the Court ruled that “the act may not be declared unconstitutional because its effect may be to accomplish another purpose as well as the raising of revenue. If the legislation is within the taxing authority of Congress—that is sufficient to sustain it.”31
On the same day as Doremus, the Court also decided Webb v. United States, which vindicated the Treasury Department’s attempts to prevent doctors from prescribing maintenance doses to compulsive users. For such a significant matter, the Court gave the issue shockingly little consideration, doing away with the argument with only a conclusory sentence: “To call such an order for the use of morphine a physician’s prescription would be so plain a perversion of meaning that no discussion of the subject is required.”32 And seemingly that was that—the Treasury Department would be able to prosecute physicians who provided maintenance doses with little pushback from the courts. By allowing Treasury agents to define a legitimate medical use, the Court essentially authorized tax agents to practice medicine.
The Webb case also highlights the inherent advantage the government has in deciding which cases to appeal to higher courts. In trying to establish precedents allowing for the prosecution of doctors who prescribed maintenance doses, the government was careful to choose those cases in which the doctor’s behavior was egregious—essentially operating “pill mills,” in today’s parlance—but who nevertheless claimed protection under the act for their supposed “medical opinions.” Dr. Webb (his first name is not reported in the decision) was clearly one of those “pill mill” offenders, as “he had been making no effort to practice his profession conscientiously with respect to addicts who applied to him; on the contrary, he simply sold prescriptions by the thousands, indiscriminately to all comers, for fifty cents apiece.”33 In other words, the government was choosing easy cases where the practice of medicine was an obvious pretense. Yet they feared the hard case: a genuine doctor with a genuine medical opinion successfully challenging the allegations and vindicating his clear right to prescribe opioids under the act.
Yet the government, in its strategizing to turn the Harrison Act’s tax and registration requirements into a de facto prohibition, blatantly misrepresented Dr. Webb’s case to the Supreme Court. The question the government asked the Court to decide was whether a prescription that was “issued for the purpose of providing the user with morphine sufficient to keep him comfortable by maintaining his customary use” fell within the act’s “professional practice” exception for opioid prescriptions.34 Note, however, that Dr. Webb’s behavior could not be characterized as “medical” by any stretch of the imagination. He was basically a narcotics dealer. That fact, more than anything, is why the Supreme Court did away with Dr. Webb’s “professional practice” argument so curtly: it was “so plain a perversion of meaning that no discussion of the subject is required.”35
Next, Dr. Moy returned to the Court, but under far more incriminating circumstances. Dr. Moy had apparently also been running a prescription-for-money service, and this time the feds had him on numerous damning charges. He sold prescriptions by weight, all to be filled at the same drugstore, and “circumstances strongly tended to show cooperation between defendant and the proprietors of the drug store.” The Court understandably ruled that the statute’s phrases “to a patient” and “in the course of his professional practice only” are “intended to confine the immunity of a registered physician, in dispensing the narcotic drugs mentioned in the act, strictly within the appropriate bounds of a physician’s professional practice.”36
Having brought and won cases at the Supreme Court featuring egregious violations of the Harrison Act that could not be reasonably called part of “professional practice,” the government now trained its sights on the next target: a physician who was not prescribing in bad faith but rather in the earnest belief that maintenance doses served a medical purpose. If the government could successfully win that case at the Supreme Court, it could establish that any prescription of opioids to compulsive users, regardless of intent or amount, was a violation of the act. For that purpose, they chose a Dr. Behrman (whose first name is not recorded in either the case caption or the Court’s opinion), who won his case at the district court before a judge who found the indictment faulty on the grounds that the Harrison Act protected the good-faith prescribing of maintenance doses.37 The government invoked the statutory right to bypass the circuit court and appealed directly to the Supreme Court.
At the Court, the solicitor general framed the question as Treasury agents wanted it: “The question, therefore, is whether every physician licensed and registered under the act is at liberty, if he honestly believes such a course to be proper, to furnish to drug addicts the means to obtain the drugs.”38 To that, Behrman’s attorney correctly responded:
The statute contains not a word of limitation upon the words “professional practice only,” nor does it use the term “addict,” or any reference whatever to any class of patients or diseases, and the Government admits that addiction is a disease. Of course, a prescription could be resorted to by a regular licensed physician as a mere subterfuge for effecting a sale. But, here, not only is there a total absence of allegation of bad faith, unlawful intent and irregularity, but language is used clearly warranting a contrary presumption in each and all of these respects.39
Yet the justices—just six of them as there were three dissenters—decided to focus on the amounts Dr. Behrman prescribed, even though the government had conceded that no bad faith was alleged. In ruling against the doctor, the six justices decided that not only would they read substantive medical standards into the statute—defining “professional practice” when the statute intentionally did not—but they would enforce their own views, rather than medical experts’ views, as to what constitutes acceptable medical practices.
In dissent, at a time when dissent among the justices was less common than it is today, Justice Oliver Wendell Holmes was characteristically clear and direct:
The defendant was a licensed physician and his part in the sale was the giving of prescriptions for the drugs. In view of the allegation that I have quoted and the absence of any charge to the contrary it must be assumed that he gave them in the regular course of his practice and in good faith. Whatever ground for scepticism [sic] we may find in the facts we are bound to accept the position knowingly and deliberately taken by the pleader and evidently accepted by the Court below.
It seems to me impossible to construe the statute as tacitly making such acts, however foolish, crimes, by saying that what is in form a prescription and is given honestly in the course of a doctor’s practice, and therefore, so far as the words of the statute go, is allowed in terms, is not within the words, is not a prescription and is not given in the course of practice, if the Court deems the doctor’s faith in his patient manifestly unwarranted. It seems to me wrong to construe the statute as creating a crime in this way without a word of warning. Of course the facts alleged suggest an indictment in a different form, but the Government preferred to trust to a strained interpretation of the law rather than to the finding of a jury upon the facts.40
Despite Holmes’s dissent, Treasury agents got their wish. What followed was, in the words of drug-war historian Rufus King, “a reign of terror.” Treasury agents began “threatening doctors who had anything further to do with drug addicts, and sending a goodly number of recalcitrant practitioners off to prison with the Behrman formula.” Any doctor would have been wise to stay away from acting on his medical opinion and prescribing to compulsive users. “The addict-patient vanished; the addict criminal emerged in his place.”41 Whereas Treasury agents had initially been charged by the Harrison Act with policing professions that provided opioids and keeping the trade visible and above ground, they now were hounding everyone and throwing thousands of people in jail, while the market for opioids began moving underground.
Narcotics agents were also seemingly abusing the indictment process, as judged by the ratio of arrests to convictions. Agents could threaten doctors all they wanted, and of course many doctors were scared enough to change their prescribing habits, but if a doctor who had been charged demanded a trial, conviction was relatively rare. In 1920, there were 3,477 arrests that went to trial but only 908 convictions. In 1921, 4,014 were arrested and taken to trial, with only 1,583 convictions.42 Charges were apparently being brought on flimsy evidence, or jurors were unwilling to convict doctors for earnestly exercising their medical judgment.
Nevertheless, as Drug War I ramped up, its human costs became evident. As of 1928, as Prohibition agents were putting axes into liquor barrels, “there were two prisoners serving narcotics offenses for every one incarcerated for liquor-law violations.” Drug offenders were 2,529 out of 7,138 total federal prisoners.43
But in 1925, the Supreme Court issued an opinion that should have stopped, or at least slowed, the Treasury Department’s war on doctors. The Court’s decision in Linder v. United States vindicated a doctor who prescribed maintenance doses in good faith, yet it did not seem to affect Treasury agents’ behavior at all, nor did it give sufficient reassurance to those doctors who feared prosecution.
The appellant, Dr. Charles O. Linder, didn’t fear prosecution, but he should have. The respected Spokane, Washington, physician was duped by an undercover narcotics agent into prescribing four tablets of cocaine and morphine. Treasury agents, as was their wont, raided his office on a Saturday, marching through a crowded waiting room and interrupting Dr. Linder while he was seeing a patient.44 He was jailed and charged under the Behrman formula and convicted. Dr. Linder did not give up, however, and took his case all the way to the Supreme Court.
This time the Court did not give the government what it wanted: an even more unfettered ability to prosecute doctors for their prescribing practices. Instead, the Court unanimously ruled that the Harrison Act protected at least some good-faith medical prescription of opioids to compulsive users. The justices were swayed by Dr. Linder’s lawyer, who argued:
It is the business of the physician to alleviate the pain and suffering of patients as well as to effectuate their cure. If we are to believe the literature on the subject, the suffering of an addict caused by deprivation of his customary drug is as intense as any suffering caused by disease. It is perhaps more so in the insistent demand for relief. Why should not the physician in the course of his ordinary practice take cognizance of that fact and administer temporary relief? It is, we submit, a strained construction of the law to hold that the language in question was intended to prohibit such an act, especially in view of the fact that the entire frame-work of the law shows that it was intended, not to regulate health and morals, but to make regulations with respect to the drug traffic which would keep it above board for the benefit of States and municipalities which do have authority and duty in that direction.45
The Court agreed, distinguishing Webb and Jin Fuey Moy as blatantly nonmedical cases of doctors simply selling prescriptions. Congress, said the Court,
may regulate medical practice in the States only so far as reasonably appropriate for or merely incidental to its enforcement. It says nothing of “addicts” and does not undertake to prescribe methods for their medical treatment. They are diseased and proper subjects for such treatment, and we cannot possibly conclude that a physician acted improperly or unwisely or for other than medical purposes solely because he has dispensed to one of them, in the ordinary course and in good faith, four small tablets of morphine or cocaine for relief of conditions incident to addiction.46
As for the Court’s previous decision in Behrman, it “cannot be accepted as authority for holding that a physician, who acts bona fide and according to fair medical standards, may never give an addict moderate amounts of drugs for self-administration in order to relieve conditions incident to addiction.”47
Dr. Linder was vindicated, but the overall victory was pyrrhic. Doctors were largely cowed into submission by zealous Treasury agents. In the words of Rufus King: “The medical profession had withdrawn completely from the field, and the doctors never permitted the addict to reapproach them. The peddler had moved in and taken over, and his profits soared as enforcement efforts kept reducing his competition and driving his customers ever deeper into the underworld, where they were easy prey.”48
For its part, the government essentially pretended that the Linder decision didn’t exist. Up until the Controlled Substances Act of 1970 supplanted the Harrison Narcotics Act, the Federal Bureau of Narcotics acted as if Webb v. United States was the law of the land. As late as 1963, Treasury regulations said this:
An order purporting to be a prescription issued to an addict or habitual user of narcotics, not in the course of professional treatment but for the purpose of providing the user with narcotics sufficient to keep him comfortable by maintaining his customary use, is not a prescription within the meaning or intent of the Act; and the person filling such an order, as well as the person issuing it, may be charged with violation of the law.49
A Path Not Taken: Restoring the Right of Doctors to Exercise Their Medical Opinions
The story recounted above is one of both a path not taken and a path that was required by the law. The medical opinions of doctors could have been respected, and opioid use, whether compulsive or otherwise, could have been regarded as primarily a medical problem.
That’s the path that Great Britain took. Although the United States in the 1920s was building a regime of de facto prohibition and imprisoning doctors, British observers looked at the U.S. system and intentionally chose another way. One British doctor who traveled to the United States in 1922 was appalled at how the country was treating compulsive opioid users:
In the United States of America a drug addict is regarded as a malefactor even though the habit has been acquired through the medicinal use of the drug, as in the case, e.g., of American soldiers who were gassed and otherwise maimed in the Great War.… In consequence of [the Harrison Act] a vast clandestine commerce in narcotics has grown up in that country. The small bulk of these drugs renders the evasion of the law comparatively easy, and the country is overrun by an army of peddlers who extort exorbitant prices from their helpless victims. It appears that not only has the Harrison Law failed to diminish the number of drug takers—some contend, indeed, that it has increased their numbers—but far from bettering the lot of the opiate addict, it has actually worsened it; for without curtailing the supply of the drug it has sent the price up tenfold, and this has had the effect of impoverishing the poorer class of addicts and reducing them to a condition of such abject misery as to render them incapable of gaining an honest livelihood.50
Britain’s Dangerous Drugs Act of 1920 was similar to the Harrison Act in that the language of the law ostensibly protected a doctor’s right to prescribe opioids in accordance with his opinion and accepted medical practice.51 Rather than allowing bureaucrats to take that language and interpret it however they wanted—as was the case with revenue agents interpreting the Harrison Act—Britain formed a committee of medical authorities to determine acceptable prescribing standards for the country’s doctors. The result was a regime that respected the medical judgment of doctors while largely preventing the creation of an extensive black market in opioids.52
Drug War II: The Modern Crusade against Doctors and Opioid Users
Today, the medical decisions of doctors are again being dictated by federal law enforcement and second-guessed by bureaucrats. The way forward is, in some way, to learn the lessons of the past. A century of mistakes in opioid policy should teach us something.
Doctors and drug manufacturers have taken the brunt of the blame for the 21st century’s opioid crisis. This often happens, as it did in the early 20th century, because of the fact—sometimes seemingly forgotten—that opioids are extremely medically useful, and in many ways, they are miracle drugs. Before the arrival of opioids, the intense pain of surgery was mitigated with alcohol and biting on sticks. Moreover, there have always been those who suffer from chronic pain, a debilitating and life-altering condition that should not be taken lightly. Yet, like any drug, there are troublesome side effects, including chemical dependence. But many drugs that help people can create chemical dependence, such as anti-epileptics, beta-blockers, benzodiazepines, and antidepressants. For millions of patients suffering through chronic or long-term pain, chemical dependence on opioids might be worth it. Yet chemical dependence on opioids is moralized differently than, say, chemical dependence on Xanax (a benzodiazepine). Addiction to Xanax and other benzodiazepines can be very serious, and managing withdrawal can be a long process of tapering doses.53 If tapered too quickly, withdrawal can directly result in death—something that does not occur with opioids. Abrupt cessation of beta-blockers such as atenolol, commonly prescribed to treat high blood pressure, can cause a hypertensive crisis resulting in a heart attack or stroke.54
Doctors are entrusted to use their medical judgment in prescribing Xanax, atenolol, and many other possibly dangerous or habit-forming drugs. Yet our century-old societal hang-up with opioid use has pushed law enforcement into the exam room.
Before further exploring how the regular practice of medicine has been criminalized, it’s worth looking at the facts and myths surrounding the modern opioid crisis.
The Mistaken Premises Underpinning Current Opioid Crisis Management
As a result of a change in the way health care practitioners address pain, the per capita volume of prescription opioids tripled between 1999 and 2015. During this same period, opioid-related overdoses reported by the U.S. Centers for Disease Control and Prevention (CDC) quadrupled. An overdose crisis was identified as overdose mortality rates reached historically high levels.
Most overdoses in the early 2000s involved prescription opioids such as hydrocodone, oxycodone, and morphine. Press reports of health care practitioners selling prescriptions and prescribing large volumes of prescriptions without obvious medical indications contributed to the narrative that the opioid overdose crisis was the direct result of health care practitioners overprescribing opioids to their patients in pain, inducing patients to engage in the nonmedical use of these drugs and causing many to develop opioid addiction.55
However, research reveals that the overdose rate from the nonmedical use of licit or illicit drugs has been increasing exponentially since at least the late 1970s—reaching dramatic levels before the end of the 20th century—and it continues unabated, with different drugs predominating as the cause of overdose fatalities at different periods.56 An examination of data from the CDC and the National Survey on Drug Use and Health reveals there is no correlation between per capita prescription opioid volume and the nonmedical use of these drugs or the development of opioid use disorder among persons age 12 and above.57 Furthermore, the National Survey on Drug Use and Health (conducted each year since 2002 by the Substance Abuse and Mental Health Services Administration) finds that the per capita addiction rate among adults has been essentially stable. Figure 1 shows survey results for the years 2002–2014. The nomenclature and wording of the survey questions changed after 2014.
As prescription opioid volume increased during the early 21st century, more prescription opioids were diverted to the underground market, where they had grown understandably popular among nonmedical users. Medically manufactured opioids with known ingredients are much less risky than black-market drugs of uncertain potency and provenance. With interventions to reduce prescription volume and diversion, largely begun around 2010, nonmedical users migrated to cheaper and more available heroin and, later, fentanyl.58 By 2019, the DEA reported that fewer than 1 percent of prescription opioids sold through pharmacies were getting diverted into the black market.59
This migration led to a dramatic surge in fatalities, as fentanyl and heroin eclipsed and then dwarfed prescription opioids as the dominant cause of opioid-related overdose deaths (see Figure 2). Most opioid-related overdose deaths involve more than one substance, including benzodiazepine tranquilizers, alcohol, and other types of opioids. Provisional data from the CDC show that illicit fentanyl, most often made in clandestine labs in Latin America and Asia, was involved in roughly 84 percent of the 73,920 opioid-related overdose deaths for the 12 months ending May 2022.60 Yet heroin was involved in approximately 17 percent of the opioid-related overdose deaths, whereas prescription opioids were involved in 19 percent. (These numbers add up to more than 100 percent because an overdose death could include any combination of fentanyl, heroin, or prescription opioids.)
The growing overdose rate from nonmedical use has fueled fears that opioids prescribed in the medical setting have a dangerously high overdose potential. That is not the case. Studies find that overdose rates from medically prescribed opioids are well under 1 percent. A prospective cohort study with a one-year follow-up of 2.2 million North Carolina patients administered opioids found an overdose rate of 0.22 percent (of which more than half involved other drugs, such as benzodiazepines, which enhance the effect of opioids).61 A major study of chronic pain patients receiving long-term opioid therapy in the Veterans Affairs system between 2004 and 2008 found an overdose rate of just 0.04 percent.62 A 2019 analysis using data provided by the Substance Abuse and Mental Health Services Administration and the CDC places the risk of unintentional non-heroin or synthetic overdoses at 0.01 percent of the population taking prescription opioids.63 The median lethal dose (LD50) of hydrocodone is 375 milligrams per kilogram in a rat (30,000 milligrams for an 80-kilogram adult, or 4,000 7.5‑milligram hydrocodone pills).64 The LD50 for oxycodone is 100 milligrams per kilogram in a rat (8,000 milligrams for an 80-kilogram adult, or 800 10-milligram oxycodone pills).65
It is also important to note that most opioid-related overdose deaths associated with nonmedical use involve multiple other drugs, including alcohol, benzodiazepines, cocaine, and methamphetamine. In New York City, 97 percent of opioid-related overdose deaths in 2016 involved more than one drug, including illicit drugs such as cocaine and methamphetamine.66 In 2017, 86 percent of opioid-related overdose deaths in New York City involved heroin or fentanyl, 49 percent involved cocaine, and just 14 percent involved prescription opioids.67 National data from the CDC reveal that 68 percent of overdose deaths involving prescription opioids in 2017 involved multiple other drugs as well.68
Government Responses to the Opioid Crisis, 2006–2019
The rise in opioid-related overdose deaths in the latter part of the first decade of the 21st century—referred to as an “epidemic” or a “public health crisis”—gained considerable public attention. The government responded on the federal and state levels.
Prescription drug monitoring programs (PDMPs), originally developed in the early 20th century, were made more efficacious by technological advances. Their proliferation was encouraged and supported by the DEA and the U.S. Department of Justice. Today they exist in all 50 states (although the Missouri PDMP is underdeveloped), the District of Columbia, and the U.S. territory of Guam.69 PDMPs serve as data banks, where all transactions involving the prescription and delivery of controlled substances are stored. They provide information regarding the frequency and number of prescriptions filled by individual patients as well as the amount and dosages of prescriptions written by providers. Federal and local law enforcement use these PDMPs to screen for health care practitioners suspected of “overprescribing” or operating “pill mills,” described as clinics operated by corrupt practitioners who have abandoned their role as health care providers in favor of simply prescribing controlled substances.70 PDMPs are also used as a tool to detect “doctor shopping” by patients who seek prescriptions for pain from multiple providers in short time spans. (As will be discussed later, some cases of “doctor shopping” are in reality pain patient “refugees” who have been undertreated or dismissed by their providers.)
Using PDMPs, law enforcement has conducted numerous raids on medical practitioners, many of whom have been indicted and sentenced to prison.71 Some have claimed that these raids are conducted indiscriminately.72 States have undertaken questionable initiatives to scrutinize providers in conjunction with medical licensing boards. For example, in 2019, California instituted the “Death Certificate Project,” in which any opioid overdose death prompted California Medical Board investigators to go back three years through the PDMP database to find any practitioner who prescribed opioids to the decedent, even if the prescription was not believed to be the fatal dose, and to consider reprimanding the provider or revoking the provider’s license.73 California physicians complained to the state licensing board that the project disrupted their ability to properly practice medicine. In late 2020, the California Medical Board changed the name of the project to the more benign “Prescription Review Project” and announced plans to look at the “entire prescription profile of the physician” during postmortem investigations.74
These interventions have cast a chilling effect on the prescribing practices of health care providers. The total number of opioid prescriptions dispensed peaked in 2012 (see Figure 3).75 Data from the National Survey on Drug Use and Health show that non-medical use of prescription opioids also peaked in 2012. The prescription rate is now below the 2002 rate, and total opioid use, including heroin, was lower in 2014 than in 2012.76 High-dose opioid prescribing (90 morphine milligram equivalents or greater) fell by 58 percent from 2008 to 2017.77 Total opioid prescribing fell 29 percent from 2010 to 2017.78 Multiple reviews of the efficacy of PDMPs have shown their association with the drop in prescription volume, but they have failed to demonstrate any effect on the overdose rate, and it has been suggested that they have directly increased the rate of overdoses from heroin.79
The Food and Drug Administration has encouraged the development of abuse-deterrent formulations of prescription opioids to prevent them from being crushed for consumption by snorting or dissolved for injecting. Considerable evidence suggests that this has only served to induce non-medical users to migrate to cheaper and more available heroin, and now to mixtures of heroin and fentanyl.80
The DEA is tasked with establishing quotas on the production of all types of prescription opioids for medical use, in all situations, allocated to individual manufacturers. This assignment presumes that a federal agency can accurately predict how many specific formulations of opioids are necessary to serve a population of 330 million people in hospital and nonhospital settings in a coming year. The agency has reduced these quotas since 2016, announcing in late 2019 plans to reduce the production of opioids to 53 percent of 2016 levels (see Figure 4).81
In 2016, the CDC issued its Guidelines for Prescribing Opioids for Chronic Pain Patients.82 In publishing the guidelines, the CDC explicitly stated that they were meant to be voluntary and “not prescriptive,” stating that health care practitioners knew their patients’ unique clinical situation and should weigh the potential risks and benefits when prescribing opioids. Many of its recommendations were based on what the CDC characterized as “Type 3” or “Type 4” evidence, which are categories of evidence that are less probative and carry a significant risk of inaccuracy. The guidelines thus came under significant criticism from many pain and addiction specialists for lacking a strong basis in the evidence.83
Others criticized the use of morphine milligram equivalents (MMEs) in determining the appropriate dosing of different opioids. As Fudin and others have argued,
MME dosing was designed in an attempt to examine opioids with similar analgesic effects and should not be used to determine an exact mathematical dosing conversion. The pharmacology and unique properties of each opioid and patient individuality must be considered when a therapeutic opioid conversion is contemplated. Conversion should not simply rely on a mathematical formula embedded within the CDC calculator software. Furthermore, the current calculation for methadone employed by the calculator could allow for potentially dangerous conversions. This is especially problematic considering this calculator is intended to target nonspecialist, general practitioners. We expect a higher level of scientific accuracy and integrity from an agency entrusted to protect citizens’ health and welfare.84
Recognizing the controversy surrounding MMEs, in August 2021, the FDA held a “public workshop” entitled “Morphine Milligram Equivalents: Current Applications and Knowledge Gaps, Research Opportunities, and Future Directions.” The workshop’s stated purpose was to “provide an understanding of the science and data underlying existing MME calculations for opioid analgesics, discussing the gaps in these data, and discussing future directions to refine and improve the scientific basis of MME applications.”85 During the workshop, Nabarun Dasgupta of the University of North Carolina Injury Prevention Research Center presented research stating: “Contrary to conventional wisdom, conversion values are not based on pharmacologic properties. Instead, they arose 60 years ago from small single-dose clinical studies in postoperative or cancer populations with pain score outcomes; toxicologic effects (e.g., respiratory depression) were not evaluated.” The research concluded: “The overlooked inconsistency among daily MME definitions revealed by our study calls into question the clinical validity of a single numerical risk threshold.… Our findings call into question state laws and third-party payer MME threshold mandates. Without harmonization, the scientific basis for these mandates may need to be revisited.”86 Some critics consider the use of MMEs to be “junk science.”87
Nevertheless, many states implemented statutory or regulatory limits on the dose (in MMEs) and number of opioids that may be prescribed to patients in acute, chronic, and postoperative situations, respectively, and they encouraged policies promoting the rapid or abrupt tapering of chronic pain patients off the opioid therapies on which they had been maintained long-term. In 2018, Oregon proposed a mandatory reduction to zero opioids in Medicaid patients over 12 months.88 The state reversed itself after receiving fierce criticism from pain management and addiction specialists.89
The 2016 CDC guidelines were adopted and cast in stone by many state regulatory agencies as well as pharmacies and health insurers. Thirty-eight states have, to date, codified CDC guidelines by imposing limits on the dosage, number, and length of time of opioids prescribed for the treatment of pain (see Figure 5).90 Repeated complaints and criticisms from the American Medical Association and from numerous health care professionals, including some who played a role in developing the CDC guidelines, led the CDC to issue a clarification against “the misapplication of the guidelines.”91 Despite the clarification, no state has revised or repealed dosage and supply restrictions.
In February 2022, the CDC published a draft of a proposed revision of its 2016 guideline that no longer promoted hard thresholds for opioid prescribing.92 However, the draft proposal still used the pharmacologically unsound morphine milligram conversion table in its methodology. The CDC accepted public comments until mid-April 2022 and is expected to publish a final revised guideline before the end of 2022.93 One of this paper’s authors submitted comments that argued that, regardless of its revisions, the CDC guideline will “inevitably become interpreted and adopted as hard and fast rules by state and local governments, pharmacies, health plans, and third-party payers, despite guideline warnings against doing so.” Furthermore, the comments contended that the CDC should not be in the business of issuing opioid prescribing guidelines. “Professional specialty organizations, overseen by practicing clinicians and clinical educators, are the institutions that should be issuing standard of care and best practices guidelines.”94
On November 3, 2022, the CDC published the final draft of the revised 2016 guideline, titled “2022 Clinical Practice Guideline for Prescribing Opioids for Pain.”95 The document emphasizes that its “recommendations related to opioid dosages are not intended to be used as an inflexible, rigid standard of care; rather, they are intended to be guideposts to help inform clinician‐patient decision‐making.” The recommendations are still primarily based on “Type 3” and “Type 4” evidence.
The guideline abandoned MME-based dosage thresholds. Unfortunately, it continued to recommend that prescribers use an MME conversion table to calculate opioid dosages. It cautioned that “before increasing total opioid dosage to ≥50 MME/day, clinicians should pause and carefully reassess evidence of individual benefits and risks. If a decision is made to increase dosage, clinicians should use caution and increase dosage by the smallest practical amount.” If the past is prologue, expect that the suggestion that clinicians use caution prescribing an opioid dose approaching 50 MME will morph into a de facto threshold mandate as lawmakers, pharmacies, and third-party payers fixate on that metric. Perhaps most egregiously, the 2022 guideline rationale remained predicated on the flawed assumption that overprescribing opioids caused the overdose crisis.96
Reacting to the 2022 guideline release, opioid policy expert and patient advocate Dr. Richard A. Lawhern commented:
Despite some conciliatory wording, the November 2022 CDC practice guidelines on prescribing opioids remain fatally flawed in basic science and medical ethics. The document profoundly over-hypes asserted “risks” of opioid prescribing. It relies on weak medical evidence, cherry-picked research, and outright junk science in 12 “recommendations” that will predictably drive even more clinicians out of pain management and more patients into suicide or street drugs.97
Finally, state and local governments have taken legal action against opioid manufacturers, accusing them of fueling the overdose crisis through aggressive marketing and by understating the overdose and addictive potential of prescription opioids.98
Criminalizing Professional Judgment
As in the 1920s, law enforcement and regulatory agencies are currently arresting or disciplining health care practitioners for engaging in what they determine to be “inappropriate” prescribing or “overprescribing,” when there is no consensus regarding appropriate prescribing in individual circumstances. Patients and clinical situations vary and are often unique, and medical experts often have diverse views on their appropriate management.
To determine when a doctor has “overprescribed,” law enforcement officials consult designated medical experts for opinions regarding the prescribing behavior of suspected practitioners based on data culled from PDMPs. Sometimes, to accumulate evidence, undercover law enforcement officers pose as patients seeking treatment for pain. To facilitate arrests for inappropriate prescribing, law enforcement agencies have an incentive to contract with medical consultants who are philosophically more conservative regarding the use of opioids. In turn, medical consultants have a financial incentive to conclude that a provider under suspicion is inappropriately prescribing.
Despite the fact that medical experts may have divergent opinions regarding appropriate prescribing in given clinical situations, law enforcement agents effectively designate the consultants’ opinions as the governing approach.
Aided by contracted medical consultants, prosecutors increasingly resort to charging doctors with homicide if they were found to have prescribed opioids believed to have been involved in an overdose death.99 Data from the Health in Justice Lab at Northeastern University show this to be a growing trend.100 Recent high-profile arrests of doctors in California, Ohio, Oklahoma, and Kansas on felony-murder charges connected to opioid prescribing further chill the prescribing of opioids by other health care practitioners.101
One board-certified anesthesiologist and pain management specialist practicing in the Midwest describes it this way:
Typically, drug trafficking and money laundering charges are a result of the illegitimate use concept, which was derived from the Controlled Substance[s] Act. The idea is to misinterpret the term “legitimate use” to mean that if an authorized medical professional disagrees with the use of the medication in the treatment of chronic pain, the targeted pain management provider can be prosecuted and charged. So if a patient has [a] back pain diagnosis (from whatever etiology), that use of a controlled substance is illegitimate if deemed not indicated, not medically necessary, or contraindicated by physicians allied with the DOJ (some well-known addiction specialists). I believe that the term “non-legitimate use” was originally intended for clearly non-medical purposes or overtly illicit purposes. These are situations where a provider traded sex for prescriptions, sold prescriptions, sold pills, etc. I do not believe that it was originally intended to prosecute physicians for disagreements over indications of treatment that others find controversial.102
This sentiment mirrors those in the 1910s and 1920s who believed that the words “in the course of professional practice only” in the Harrison Act were intended to focus on obviously illegitimate prescribing practices such as true “pill mills,” where prescriptions are sold without medical consultation. Doctors who prescribe opioids within the scope of legitimate medical judgment (as determined by a representative sample of their peers rather than by specially chosen witnesses for the prosecution) should be protected as acting within their “professional practice.”
What Defines “Overprescribing”?
Creighton University professor Kelly K. Dineen Gillespie points out that “no other decisions in medicine risk such a breadth of legal scrutiny as opioid prescribing, which elicits fear and avoidance.” Yet explicit definitions of “overprescribing” or “inappropriate prescribing” are rare.103 One definition of inappropriate prescribing in the context of multiple medication use in the elderly—but not in the context of opioid use—is provided by Polona Selic and others:
Inappropriate prescribing means the use of a drug for which the risk of [adverse drug events] outweighs the clinical benefits, and which could result in harmful effects, either through interactions between drugs or through the non-use of a drug with proven efficiency for patients with sufficiently long life expectations and a good quality of life.104
Gillespie’s review of the legal literature found that no definitions of inappropriate prescribing were found in legal or public policy contexts. The Controlled Substances Act allows for the prescription of opioids for “a legitimate medical purpose” in “the usual course … of professional practice.”105 The DEA’s Practitioner’s Manual discusses “inappropriate prescribing” in the context of criminal prescribing:
While there are no criteria to address every conceivable instance of prescribing, there are recurring patterns that may be indicative of inappropriate prescribing: an inordinately large quantity of controlled substances prescribed or large numbers of prescriptions issued compared to other physicians in an area; no physical examination was given; warnings to the patient to fill prescriptions at different drug stores; issuing prescriptions knowing that the patient was delivering the drugs to others; issuing prescriptions in exchange for sexual favors or for money; prescribing of controlled drugs at intervals inconsistent with legitimate medical treatment; the use of street slang rather than medical terminology for the drugs prescribed; or no logical relationship between the drugs prescribed and treatment of the condition allegedly existing.106
In response, Gillespie writes:
This implicit definition addresses corrupt prescribing only. However, the patterns they list do not necessarily correlate with corrupt or criminal prescribing. In particular, “inordinate” amounts depend upon context and prescriber specialty. On the other hand, some are squarely within the criminal standard, such as exchanging prescriptions for sexual favors or money.107
The Food and Drug Administration refers to “careless prescribing” but does not define inappropriate prescribing. The Center for Medicaid and CHIP Services tracks “inappropriate prescribing” through the lens of patients/recipients receiving high-dose prescriptions, or prescriptions from multiple providers or pharmacies. Similar tracking measures were recently implemented by the Center for Medicare and Medicaid Services to track Medicare beneficiaries, focusing disproportionately on chronic pain patients.
The Substance-Use Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) Act of 2018 authorized grants to use PDMPs to detect inappropriate prescribing, but again it did not define inappropriate prescribing. Section 6902 of the SUPPORT Act directs the Department of Health and Human Services to develop guidelines for opioid prescribing to hospitalized patients but, again, does not define overprescribing.
Recognizing the absence of a legal definition for overprescribing, the Nevada legislature defined overprescribing as “prescribing outside of the standard of care for a prescriber’s practice, specialty, or medical need of the patient” and ordered its state licensing board to set those standards. The standards have yet to be set.108 Florida doesn’t define appropriate prescribing practices, but it nevertheless requires providers to be educated on the standards; Maine just decided to adopt the inadequate CDC guidelines; and Texas says inappropriate prescribing “may lead to or contribute to abuse, addiction, and/or diversion of drugs,” yet it doesn’t define the vital terms “abuse” and “addiction,” much less the stunningly vague phrase “may lead or contribute to.”109
As Gillespie points out, these inconsistencies and the lack of clarity lead to “overcorrection and fear by providers and other stakeholders.” Those may lead to abrupt tapering or outright discontinuation, chasing patients to the black market or to suicide.
Michael E. Schatman and Stephen J. Ziegler understandably ask:
So, what amount of prescribing is appropriate? This represents a difficult question since one size does not fit all. A particular type or dose of one medication may be appropriate for one patient and condition and wholly inappropriate for someone else. Yet despite the medical necessity of tailoring treatments to the individual, the tendency today is for an across-the-board reduction in prescription opioid availability.110
Gillespie concludes her review thus: “To date, no policy, law, or guidance defines inappropriate prescribing. This leads to policy development and evaluation not guided by evidence but by bias and oversimplification.”111 Like obscenity, law enforcement apparently knows “inappropriate” prescribing when it sees it.
Aided by PDMPs and paid medical consultants, law enforcement continues to arrest doctors for overprescribing and terrorizes others into underprescribing, rapidly tapering, or abandoning pain management altogether. This amounts to the de facto establishment of standard-of-care criteria for the management of pain by agents of law enforcement using capricious and arbitrary definitions of “inappropriate prescribing.”
In light of more than a century of terrorizing doctors for using their medical judgment in a manner deemed illegitimate by law enforcement, it is time for a new regime to determine the criminal liability of medical professionals accused of misprescribing opioids.
“Overprescribing” Opioids Is a Standard-of-Care Issue, Not a Crime Issue
Among the characteristics that distinguish the biological sciences, including medical science, from the physical sciences is that living organisms respond in diverse and variable ways. Whether a disease has external or internal causes, its manifestation and expression can vary widely among organisms of the same species. Responses to therapeutic interventions can vary as well. That is why multiple pharmaceuticals are developed to treat the same problem. Some patients will respond favorably to one medication that may have no effect on other patients who have the same condition.
A classic example is high blood pressure. Drugmakers continue to develop new anti-hypertensives with various mechanisms of action. Some patients’ blood pressure will be brought under control by one class of drug—say, a beta-blocker—while for others an angiotensin receptor antagonist may work better. Some may require combinations of drugs to get their blood pressure under control. In many cases, a hypertensive medication regimen will need adjustments in dosing or complete revision over time.
Undoubtedly, there are some clinicians who mismanage their patients’ therapeutic regimens. Sometimes mismanagement can lead to serious, even fatal consequences. One remedy is the civil tort system. But the raison d’être of professional licensing boards is to enforce the “standard of care” rendered by the professionals they oversee.112 According to Peter Moffett, MD, and Gregory Moore, MD, JD, the standard of care is defined as “what a minimally competent physician in the same field would do in the same situation with the same resources.… Clinical practice guidelines are being used more frequently in court cases as support for the standard of care; however, their acceptance and uses are continually changing and decided on a case-by-case basis.”113
Whether the issue is overprescribing or inappropriately prescribing antibiotics, psychiatric medications, or anticoagulants, licensing boards are responsible for enforcing the standard of care.114 When concerns arise regarding a practitioner meeting the standard of care, an investigation is initiated by peer professionals who understand the variability and nuance of treating medical conditions. Practitioners who deviate from the standard of care are educated and disciplined accordingly. In some cases, licenses may be restricted or revoked.
The treatment and management of acute and chronic pain involves the same nuanced medical decisionmaking as does the treatment of hypertension, diabetes, infectious diseases, and psychiatric disorders. For example, it is not necessarily inappropriate for physicians to renew opioid prescriptions for patients with whom they have long-standing clinical relationships after a cursory conversation, without performing a physical examination. Prescribing conduct that might be interpreted by non-physicians as being consistent with “pill mill” behavior might be seen by medical board physician-reviewers as clinically appropriate.
There is no justification for law enforcement personnel, untrained in the health sciences, to intervene in a matter for which health professional licensing boards were created. Inappropriate management of pain, like inappropriate management of hypertension, is a concern for the licensing boards to address.
Conclusion
Drug use and substance use disorder should be viewed as health issues, not crime issues. Law enforcement has no expertise and should have no say in classifying narcotics and psychoactive substances.
The following are some recommendations to policymakers:
States should resist efforts to codify any new guidelines released by state and federal public health agencies. By their nature, guidelines are suggestions based on the state of knowledge—often observational and inconclusive—at the time the guidelines were published, and they are constantly subject to revision as new knowledge is gathered. Guidelines recognize that one size does not fit all, and that individual context matters—which is why they always are considered a rule of thumb as opposed to absolute instructions. Codifying guidelines has the effect of casting them in stone; it makes nuance impossible. It incentivizes law enforcement agencies to view any deviation from the guidelines as a legal transgression and, as a result, frightens practitioners into abiding by the guidelines at the expense of their best medical judgment.
The DEA should no longer be empowered to impose manufacturing quotas on opioids. The agency has been given the impossible task of determining the number of opioids, of all categories, that a population of more than 330 million people will need for pain management in the coming year.
All physician prescribing behavior considered suspicious by law enforcement should first be reviewed by state medical licensing boards before any action is taken against the prescriber. Medical boards have expertise in distinguishing appropriate versus inappropriate prescribing, whereas law enforcement agencies lack that expertise.
Medical boards have the authority to revoke licenses, as well as to refer doctors to relevant agencies for criminal investigation. If the licensing board concludes that the prescriber in question failed to meet the standard of care, it will take appropriate disciplinary action. Board investigations revealing possible criminal statutory violations should then be referred to law enforcement.
The use and possible misuse of narcotics and psychoactive drugs should never have been matters for law enforcement. They have always been private and public health issues. Just as armed agents of the state don’t break down doors and arrest people for (inappropriately) self-medicating for a viral illness with antibiotics, they should not do so to those who self-medicate for pain or even for pleasure with opioids or other psychoactive drugs. Neither the practice of medicine nor the act of self-medication belongs in the realm of the criminal legal system.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.